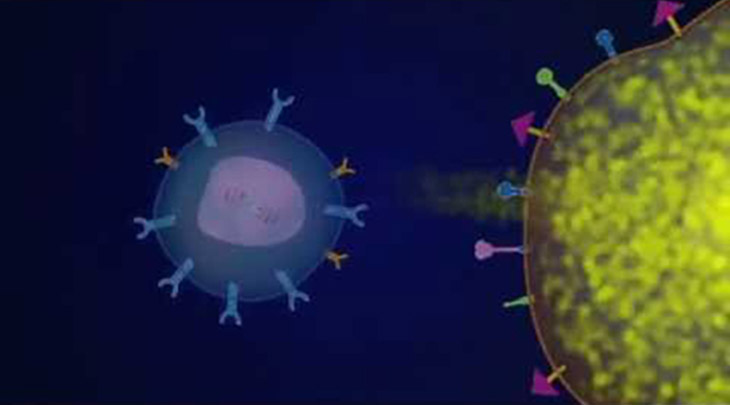
Immunotherapy is a type of cancer treatment which assists the body’s immune system to fight cancer. Cancer cells can suppress immunity, which may contribute to the immune system’s failure to recognize cancer cells as foreign invaders.
There are many different ways that immunotherapies work to help our immune systems recognise and kill cancer cells.
Overview of immunotherapy
Immunotherapies can also be known as ‘targeted therapies’ or ‘biological therapies‘. This is because they target different parts of the immune cells, pathways that allow the cells to grow and divide.
The immune system can then continually adapt to the cancer over time and provide a durable, long term response to the cancer. The immune cells called antibodies can remember, recognize and kill cancer cells in the future.
How do they work?
There are different kinds of immunotherapy and they work in different ways. Immunotherapy can boost the immune system to work better against cancer or remove barriers to the immune system attacking the cancer.
Immunotherapy takes advantage of a person’s own immune system to help kill cancer cells. Immunotherapy treatments help fight the lymphoma by giving the immune system a long-lasting memory.
Immunotherapies can be given as a single treatment or it can be given in combination with chemotherapy, called chemoimmunotherapy.
When are they used?
Immunotherapy treatments are used for lymphoma types which have been shown to respond to them.
Immunotherapy is not suitable for everyone. The doctor will consider:
- Overall health
- Lymphoma subtype
- If the lymphoma has spread (the stage)
- Treatment history
Types of immunotherapy
Antibody therapy
There are different types of antibody therapies that work slightly differently. They are known as monoclonal antibodies, bispecific monoclonal antibodies and include antibody drug conjugate therapies. There are immune system proteins created in the lab that are designed to bind to specific targets on cancer cells. Some antibody therapies mark cancer cells so that they will be better seen and destroyed by the immune system. Some examples of antibody therapies include:
- Rituximab (MabThera)
- Obinutuzumab (Gazyva)
- Ofatuzumab (Arzerra)
- Brentuximab vedotin (Advertis)
- Polatuzumab (Polivy)
- Alemtuzumab (Campath)
- Mosunetuzumab
What are the common side effects of immunotherapy?
Side effects from immunotherapy can vary depending on the type of treatment that has been given and how the patient’s body responds. The side effects of checkpoint immunotherapy are different from those of other cancer treatments.
Common side effects include:
- Fever
- Chills
- Weakness
- Dizziness
- Nausea or vomiting
- Fatigue
- Shortness of breath
- Headache
- Low or high blood pressure
- Muscle and joint pain
Common immunotherapies used for some lymphoma subtypes
Below is a sample of some of the common subtypes of lymphoma and some of the monoclonal antibody and targeted therapies that are either currently being used in Australia (in bold) or are currently being investigated in clinical trials .
Subtype of lymphoma | Medicine |
Chronic lymphocytic leukaemia (CLL)/small lymphocytic leukaemia (SLL) | Obinutuzumab Ofatuzumab Rituximab Ibrutinib Idelalisib Venetoclax Acalabrutinib Zanubrutinib CAR T-cell therapy Mosunetuzumab |
Diffuse large B cell lymphoma (DLBCL) | Rituximab CAR T-cell therapy Polatuzumab Lenalidomide
|
Follicular lymphoma | Obinutuzumab Rituximab Ibrutinib Idelalisib Lenalidomide CAR T-cell therapy |
Hodgkin lymphoma | Pembrolizumab Brentuximab vedotin Nivolumab CAR T-cell therapy |
Primary mediastinal B-cell lymphoma | Rituximab Pembrolizumab CAR T-cell therapy |
Mantle cell lymphoma | Rituximab Ibrutinib Lenalidomide venetoclax Zanubrutinib Acalabrutinib Mosunetuzumab Umbralisib CAR T-cell therapy |
Marginal zone lymphoma | Rituximab Ibrutinib Idelalisib Umbilisib Lenalidomide |
Skin lymphoma | Brentuximab vedotin Romidepsin Vorinostat |
Systemic anaplastic large cell lymphoma | Brentuximab vedotin |
T-cell lymphoma | Brentuximab vedotin Lenalidomide Romidepsin Belinostat |
Waldenström’s macroglobulinaemia | Ibrutinib Idelalisib Bortezomib Acalabrutinib Zanubrutinib |
Dr Michael Dickinson, Lead for aggressive lymphoma, Peter MacCallum Cancer Centre
Dr Michael Gilbertson, Monash Health
Prof John Seymour, Director of Haematology, Peter MacCallum Cancer Centre
Prof John Seymour, Director of Haematology, Peter MacCallum Cancer Centre
Prof Constantine Tam, Lead of indolent lymphoma, Peter MacCallum Cancer Centre
A/Prof Chan Cheah, Sir Charles Gairdner Hospital, Hollywood Private Hospital & Director of Blood cancer WA
Dr Michael Dickinson, Lead for aggressive lymphoma, Peter MacCallum Cancer Centre
Dr Ken Micklethwaite, Westmead Hospital

